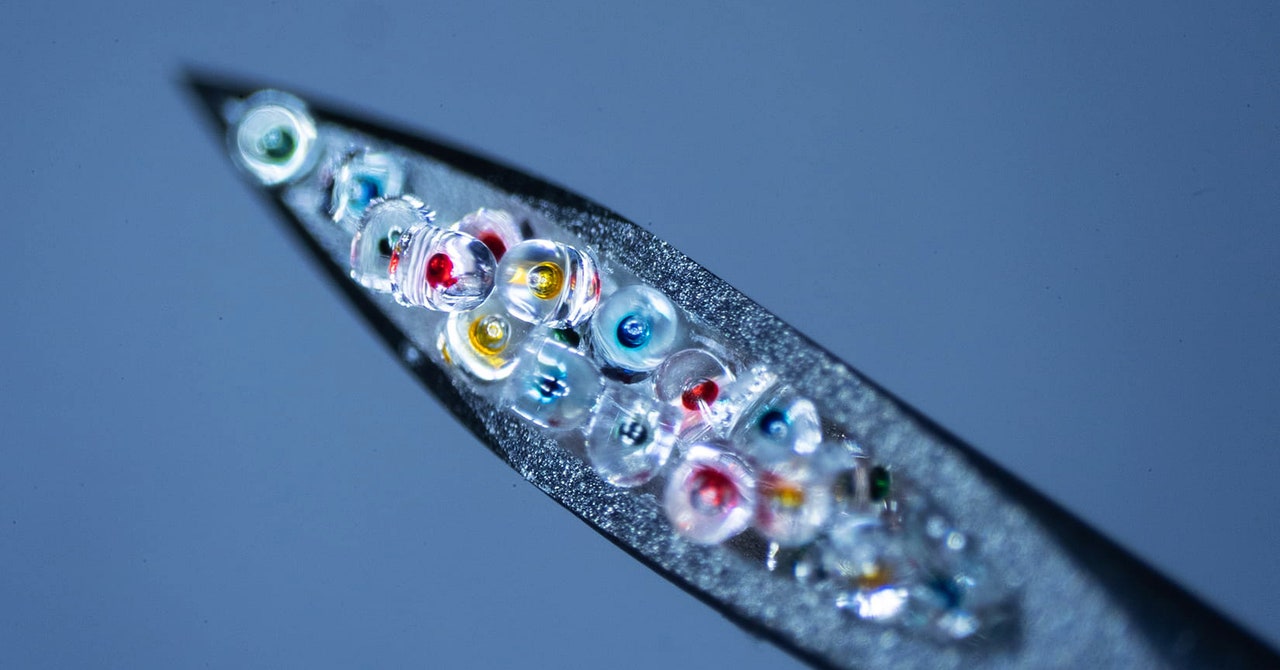
Today they use lab robots to fill the capsules, and they are working to automate the entire process, which they call Pulsed, for Particles Uniformly Liquified and Sealed to Encapsulate Drugs. McHugh believes that this automation cuts costs and makes the tech scalable. Thanks to minor tweaks to the capsule recipe, the Pulsed particles rupture with distinct, predictable delays, ranging from days to over a month.
For their recent study, their team wanted to know how quickly these capsules would degrade in a living animal, so they compared the timing in test tubes to that in mice. In one trial, they loaded the microparticles with tiny fluorescent molecules in lieu of medicine. With the mice, they injected a small volume of the capsules beneath the animals’ skin, then they tracked the fluorescence as the molecules diffused outward. With the test tubes, they kept the capsules in a saline solution at body temperature and checked to see when the fluorescent molecules spilled into the solution. In all cases, the timing matched. This means that timing predictions based on lab experiments will likely hold up well in living bodies.
They also tested whether the microparticles can carry biologics without spoiling them. They tested one—bevacizumab, the antibody that treats macular degeneration and some cancers—by loading the drug into microparticles along with a cocktail of stabilizing chemicals. Eighteen days later, the drug remained over 90 percent active.
The team envisions designing a library of these particles that can mimic different dosing schedules: daily, weekly, monthly, or something in between, depending on the patient. For example, while they haven’t yet tested their system with Covid vaccines, the capsules described in the new study could match the timing needed for them: two doses given at three- or four-week intervals.
“It’s really an important direction for the future of controlled and sustained drug delivery,” says Kibret Mequanint, a biomedical engineer with the University of Western Ontario, who was not involved in the work. However, he points out, the current particles are not ideal for drugs that require doses multiple times per day—they don’t dissolve fast enough.
Compared to other injectables or slow-release oral pills, the microparticle results are “very exciting,” says Rahima Benhabbour, a polymer chemist at the University of North Carolina who is not involved with McHugh’s team. “The main takeaway here is the stability of the biologics. I really liked that,” she says.
Benhabbour’s team uses PLGA to create implants that release drugs at a slow and steady rate, with no initial burst. (Drug levels from injections typically spike before tapering down.) That’s essential for HIV pre-exposure prophylaxis, or PrEP, which requires a person to maintain a certain concentration of the drug in their bloodstream at all times to be protected. Her team published a paper in February reporting that, based on tests in macaques, their implants could maintain those PrEP concentrations in people for over five months.
Benhabbour cautions that it’s unclear how many microparticles could be squeezed into one injection. The maximum volume for subcutaneous injections for humans (like those given to McHugh’s mice) is 1.5 milliliters. That’s not guaranteed to be enough space for multiple doses, especially drugs like PrEP that require a lot of medication per dose. “The only question I have is: Can they deliver enough?” she says.

