In February, a 23-year-old Tanzanian fisherman suddenly fell ill, having just returned from a busy trading outpost in the middle of Lake Victoria. Back at home in Bukoba, a district in northwestern Tanzania, he was hit by bouts of vomiting and diarrhea. He developed a fever and began bleeding from his body openings. On March 1, he died.
His family and community conducted a routine burial—not knowing this gathering would be the beginning of a deadly outbreak. Soon, some of those present began to fall ill. On March 16, Tanzania’s chief medical officer announced that an unknown, “possibly contagious” illness had been detected and deployed a rapid response team to Bukoba. Finally, five days later, PCR testing at Tanzania’s National Public Health Laboratory revealed the cause: Marburg virus.
This wasn’t the first appearance of Marburg this year. On February 13, Equatorial Guinea reported its first ever outbreak. A deadly virus, spreading in new places on opposite sides of the continent at the same time, is a big warning. It shows not just the ever-present threat of viruses spilling over from nature into humans, but that, yet again, the world isn’t prepared to deal with these dangers.
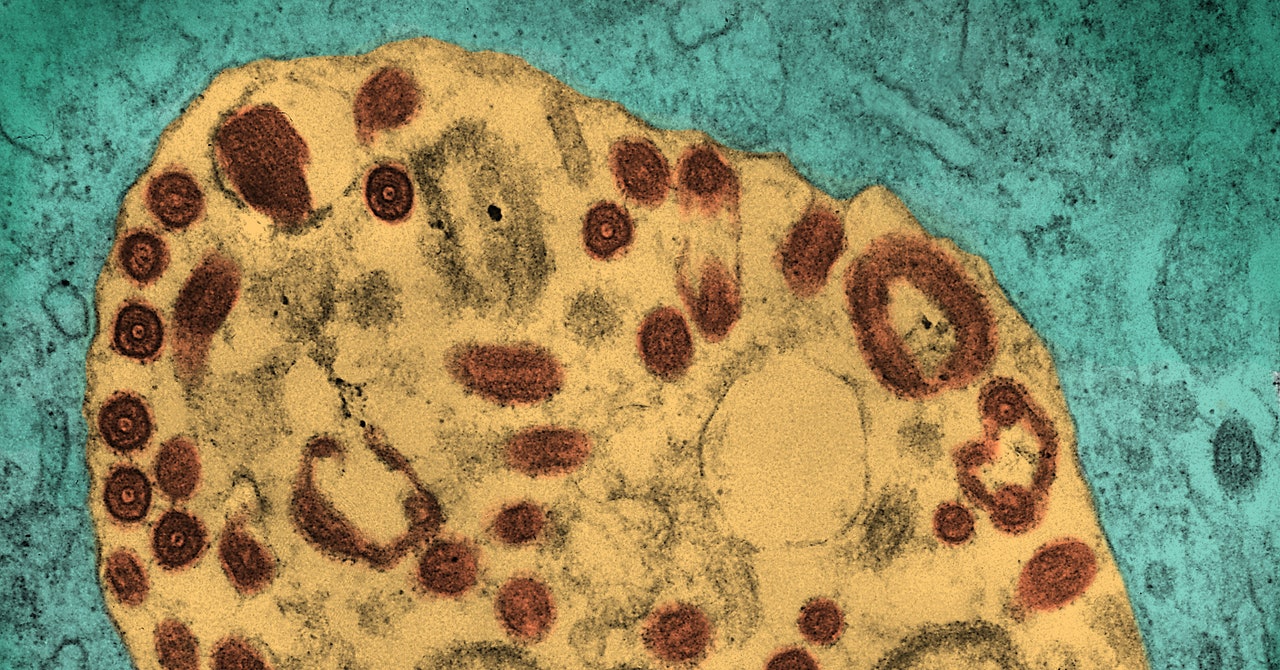
Marburg shares plenty of characteristics with Ebola—the viruses are part of the same family. Like Ebola, it causes viral hemorrhagic fever, resulting in dangerous internal bleeding and organ damage. In some outbreaks, up to 90 percent of cases have been fatal; at the time of writing, five of the people in Tanzania’s eight confirmed cases have died. Symptoms take anywhere from a few days to three weeks to develop, and the virus can spread through human contact, particularly via body fluids of an infected person or corpse. Fruit-eating bats of the Rousettus family are the virus’s suspected host.
So similar are the symptoms that “in this village, most people believe it’s Ebola,” says Abela Kakuru, a resident of Ibaraizibu, which is a 10-minute drive from Bukoba’s affected villages. But there’s one big difference: Unlike with Ebola, no vaccines or antivirals have been approved for Marburg. Fluids, electrolytes, blood, and oxygen can be given to treat the symptoms, but there’s nothing yet to contain or fight the virus. “Supportive care to patients is the mainstay of treatment,” Tanzania’s minister of health, Ummy Mwalimu, said in a press briefing in late March.
Developing a vaccine thankfully doesn’t have to start from scratch. Several experimental vaccines have shown promise in nonhuman primates, and one from the Sabin Institute has also recently been tested in a small number of humans. It was found to be safe and to stimulate an immune response.
The World Health Organization is now planning to start trials of some of the experimental vaccines using what’s known as ring vaccination. “It means we will offer the vaccine to the close contacts of the cases,” says Ana-Maria Henao Restrepo, co-lead of the WHO’s R&D Blueprint for epidemics. “This is, in our experience, about 20 to 50 people, depending on the social network of each case.” Statistical analysis of how many contacts subsequently become infected should allow researchers to calculate how well the vaccines work.


